 Unfortunately, I had to neglect my blogs for some considerable time due to disease and pressure from my businesses. This has been very frustrating for me but I really had no choice, my work pays the bills and I had reached the point where I was working twelve to fourteen hours every day, including weekends.
Unfortunately, I had to neglect my blogs for some considerable time due to disease and pressure from my businesses. This has been very frustrating for me but I really had no choice, my work pays the bills and I had reached the point where I was working twelve to fourteen hours every day, including weekends.
Due to the additional stress from work I strayed from my diet and became very ill. I had huge problems with my knees and this triggered inflammation in many other joints too.
Unfortunately I had to keep working on-site and away from my office and home, so I began to eat and drink things which I knew would cause problems, but at the same time I needed the energy and often the caffeine too :-)
Eventually I reached the point where I needed to have cortisone injections in my knees again, in order to continue working. I kept saying to myself, I will just get on top of things then go back to my diet and recover but new problems kept getting in the way.
The Original Cause of my Rheumatoid Arthritis – Discovered in Turkey!
As it happens, I recently went to Turkey to be with my mother-in-law (actually anneciğim in Turkish) because she was about to have a major operation. Unfortunately I was still ill myself and I became worse on the journey due to the flights, airports, taxis and such.
The first few days there I was very ill and had to go to hospital for treatment. While waiting for mum’s exact operation date to be confirmed, I also saw several other doctors myself regarding my RA (mostly friends of the family). This is where it got interesting!
I will write in more detail about my visit and the things I discovered there later, but in a nutshell; I discovered one of the original causes (possibly the only/main cause) of my rheumatoid arthritis :-)
The Turkish medical system is very flexible and responsive, and tests results & X-rays can be obtained almost immediately. As a result I was able to accumulate useful test results, scans and expert opinions in a very short timescale – just a few hours.
It was soon explained to me that I had a long standing blood infection that required urgent treatment; systemic inflammatory response syndrome – a kind of sepsis which can be fatal. My doctors there were amazed that I was still alive and equally amazed that I had managed to fly to Turkey in such a condition. They arranged for me to be admitted to hospital for treatment and monitoring and I started taking oral antibiotics soon after an initial intravenous injection.
After discussing the history of my symptoms and studying my many new test results they concluded that I had probably had this infection to some degree for at least the last twenty-five years, but that it was currently life threatening. If I had not gone to Turkey, I would perhaps never have realised the serious state of my disease and would have continued to believe that my symptoms were just a flare-up of my existing RA – and possibly died.
My RA Caused by Tooth Infection Missed by Doctors and Dentists
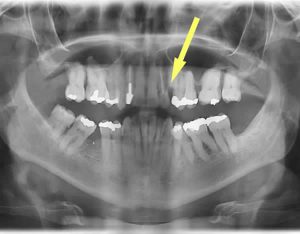
I was immediately given powerful antibiotics and then referred to a dental surgeon in a local specialist hospital (another family friend) as my doctors suspected a long standing tooth abscess was the original source of the infection. In our discussions, I explained that I had had a problem tooth for about thirty years and that it often caused pain, bad breath and various other symptoms. I also explained that I had brought it up with several of my UK GPs over the years but that they had always dismissed it as a possible cause of my RA and had not considered it to be a serious problem. Unfortunately, after several soul destroying attempts to obtain dental treatment in the UK, I eventually gave up and just accepted the pain. Had I known the extent of the problem, I would have persevered of course and obtained treatment, somehow.
The dental surgeon confirmed my doctors’ suspicions with the help of various scans, examinations and blood tests. Again, he could not believe the extent of the infection and explained that it was difficult for him to remove the problem tooth in my current condition as it was too badly infected. He prescribed additional specific antibiotics to complement the ones obtained from my doctors and asked me to call in periodically to monitor my progress. He also shared his findings with my doctors.
A few days into taking the antibiotics, my symptoms started to improve, particularly in my mouth of course but also I noticed a greater range of movement in some of my fingers and my feet were no longer swollen. A week later whilst discussing new blood test results with my doctors, they confirmed that I had achieved about a 30% improvement in the severity of my infection (apparently enough to silence the alarm bells). Following on from this, they advised me that it would take between one and three years of oral antibiotic treatment to completely clear the infection, along with appropriate dental treatment. My doctors also explained that intravenous antibiotic therapy would be more effective but since I was only there for a short time, it wasn’t really practical because I wouldn’t be able to continue the treatment in the UK.
The upshot of all this is, I have proof of what I always suspected to be the case; that my joint inflammation was caused (in part or wholly) by some type of infection, and now I know what it was and how it started; a streptococci group – tooth/gum infection which gradually became a hidden abscess inside my gum/jaw where most of the infected tooth broke away and left a deep hole which never healed.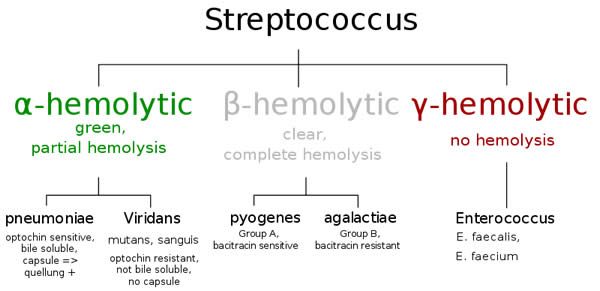 Streptococcus mutans causes plaque, tooth erosion and cavities and this was probably what initiated my problem decades ago. However, my systemic infection appears to have been caused by group A or B streptococcus originating either directly from my long-term tooth infection/abscess, or by external infection from some contaminated food or drink due to the susceptibility of my broken tooth and the deep surrounding abscess. Unfortunately, because of the rush to administer antibiotics and because I was feeling so ill, I never managed to obtain further more detailed tests to confirm exactly which strain caused or worsened my joint inflammation. However I suspect ‘pyogenes’ because of my symptoms; swollen lymph nodes, intermittent fever, increased joint inflammation, flu symptoms, skin rash etc.
Streptococcus mutans causes plaque, tooth erosion and cavities and this was probably what initiated my problem decades ago. However, my systemic infection appears to have been caused by group A or B streptococcus originating either directly from my long-term tooth infection/abscess, or by external infection from some contaminated food or drink due to the susceptibility of my broken tooth and the deep surrounding abscess. Unfortunately, because of the rush to administer antibiotics and because I was feeling so ill, I never managed to obtain further more detailed tests to confirm exactly which strain caused or worsened my joint inflammation. However I suspect ‘pyogenes’ because of my symptoms; swollen lymph nodes, intermittent fever, increased joint inflammation, flu symptoms, skin rash etc.
This of course makes me think that there could be many more people out there suffering with rheumatoid arthritis or other inflammatory conditions, who may have a tooth related infection (there appear to be three types of tooth/gum abscesses) and who may not realise its importance as a potential cause of their disease.
I want to recommend that if you have any kind of tooth decay/pain/abscess and also suffer from RA, get your teeth looked at and get any problems fixed straight away, even if like me you have been putting it off or putting up with it. Also, if you do a little research, you will quickly find a number of papers and articles like this one confirming the link between abscess infection and rheumatoid arthritis and this example of a link between a dental streptococcal infection and rheumatoid arthritis.
![]() “Streptococcus” image is public domain
“Streptococcus” image is public domain ![]()
Do have any names of the tests the Turkish doctors performed???
I’ve been trying to convince different doctors for the past decade to do further testing on me for infections, as my RA started 3-4 months after a double root canal in same tooth!!
No doctor listens!!! I am finally just going to get my tooth removed, but I would want to know what antibiotics to eat to get rid of this infection.
Hi Nida, thanks for your comment.
The tests that I had carried out in Turkey were general blood panel tests which included; ESR, CRP, Rheumatoid factor, and a few other markers which can be used to assess systemic infection. Unfortunately, I can’t remember the specifics.
I can confirm that a tooth infection is likely to have an effect on the severity of your rheumatoid arthritis symptoms. It’s definitely a good idea to have the tooth treated or removed if necessary. I would follow the advice of your dentist regarding any antibiotics that may be required.
Unfortunately I can’t give any specific medical advice and the antibiotics that were used in my case may not be applicable to yours. However, I can suggest an area which you can research and then subsequently discuss with a Lifestyle Medicine based doctor such as Dr Klaper who does Skype-based consultations.
The Antibiotic Protocol for Rheumatoid Arthritis (Halfway down the page).
https://www.doctorklaper.com/contact
I finally got my root canal tooth removed and another tooth which was dead. Both showed infection in the x-rays, had bone grafting done also
Now I’m waiting n seeing what improvements I feel with my joints.
I am on normal antibiotic… No extra pain killer. Only paracetamol. ( I have never taken RA meds over the past 11 yrs)
So far, day 1 after teeth out… I’m feeling 70% Less pain in knees n elbows. I went up n down stairs a couple of times, and stood up cooking for more than an hour. I have not been able to do that in more than a year!!! Def a positive sign. Thank God!!
Hoping the return of health continues!!
Hi all. I’m in the uk, with a very complicated medical history and a severe dental phobia, what I would consider a “real” phobia as opposed to a irrational fear.
I have Elhos Danlos (a genetic inherited connective tissue disorder, think almost dislocating, called subluxating), I’ve had life long joint problems and multiple pain sights. A symptom of EDS is a high tolerance to local anesthetics, I’ve literally had years of telling dentists i feel pain…sigh….with them telling me I can’t! After 30 years i was diagnosed, however I have become phobic.
6 years ago a year after the death of my partner, I awoke to a rheumatoid flare and unable to move, quite terrifying as I live alone! I had an appointment to have a tooth removed in the hospital a week later, pre op, as I had a chat underneath it, but, due to the steroids tablets and EDS, the dentist wouldn’t operate until I had come off the steroids, it took a whole year and I was weaned off steroids and into methotrexate. I’ve also been diagnosed with fibromyalgia, under active thyroid, b12 and D deficiencies, a recent 1 1/2 cm gallstone and non alcoholic liver disease (which is caused by the methotrexate, which I’ve had to stop so my liver can heal)
I know I should have gone back for dental treatment but I put it off, I’m world class at procrastinating. So here I am, with a cyst under an upper tooth, plus I now have an abscess under my last lower molar. This is why I found this post, I’m wondering why none of my rheumatologists have put this together!
Due to covid-19 and my immune system being suppressed I’ve been at home since the end of February, in which time my lower molar has abcessed 3 times! I’ve got amitriptyline (which really does help with abscess pain) for fibromyalgia. After reading this though, I’m determined to get on the phone to the doctor in the morning, I’m at the point where I want all of my teeth removed and I’m annoyed at the lack of interest and investigation from the rheumatology dept, I’ve had 6 years of constantly high esr and crp blood tests, every month for 6 years!!😡😠
Please can you give me the clinic on private message? I have jaw infection after tooth removal and since then I can barely walk… I’m sure everything started with the problematic tooth and a dental granuloma under but cannot get adequate treatement. I’m seriously considering to go to Turkey (I live in Bulgaria) for diagnosis and treatment .
Hi Svetla, I didn’t visit a particular private clinic it was just a local hospital where I attended as a private patient in Turkey and they helped me a great deal. Later I had the infected tooth removed by a local dentist in the UK. I still don’t have a particular dentist that I’m comfortable with and I’m still searching. However, I can give one piece of advice; Look for a dentist that uses a device called a ‘magic wand’, it’s a painless method of applying local anaesthetic and helps a great deal with the procedure. Another suggestion I would make since you have an infection, is to visit your local hospital as an out-patient and ask them to take a look at your jaw. Even if they’re not able to carry out the actual dental treatment there and then, they will be more capable of identifying and treating the infection.
I am 57 and I just went through this the past month. I cracked my 2nd to last molar and left it in for 3 weeks. Over the 3 weeks my right knee got so swollen I could not walk, had X-rays, an MRI and nothing was detected. I had my knee drained last week and a cortisone shot too. I was put on a high dose of anti inflammatories for my knee. I have also been on Anti Biotics for my extraction and bone graft in my mouth 10 days ago. The knee surgeon called today and said knee is structurally great. It is also coinciding with the 10 days out from the tooth extraction and bone graft.
If you have one joint swollen unable to move make sure you check to see if you’re tooth is cracked anywhere. I was the source of my pain.
Hi Paul, thanks for your comment and your valuable advice regarding the link between teeth and swollen joints. It’s great to hear that you found the connection between your tooth and your knee inflammation.
i hve seen 40 improvement and still improving after removing root canal tooth.i got my tooth removed 7 months ago.thnq u internet to give me d clue about my RA
Hi Pooja, thanks for your comment. It’s great to hear that you are improving after your tooth removal. :-)
I very recently had an 11 year old root canal molar removed after being diagnosed with RA 6 months ago. The tooth was not bothering me other than slight sensitivity occasionally and did not look bad on dental X-rays, but had some nasty stuff underneath it when removed. I have stopped taking my methotrexate and plaquinil, but continue to take vitamins and maintain my diet. So far, my pain has completely stopped on some days and was only mildly painful on days when rain was predicted. The tooth was removed a week ago…I am praying that these results continue.
That’s excellent news! Thanks very much for posting :-) it must have been a difficult decision to make and I’m glad it had such a beneficial outcome for you. Unfortunately that’s often the case, x-rays don’t always show underlying infection. I’m considering having one of my molars removed for similar reasons; simply because of a suspicion of hidden infection. I’m so glad you were able to stop your medication and manage with your healthy diet alone. I’m sure your recovery will continue :-)